- March 3, 2023
- By: Dr. Subodh Kamble
- No Comments
WHY UROLOGIST SHOULD LOOK INSIDE THE BLADDER!
Cystoscopy in patients with Overactive bladder (OAB)
In my practice I mostly get patients with complex urinary problems who had tried several urologists all over and had several treatments before. Many of my patients have neurological bladders as well, which can be extremely complex condition to treat. Every day I receive several calls from patients or their relatives not only from many parts of Gujarat and Maharashtra but also from UK and USA. For such patients a diagnostic Cystoscopy (some people call it a telescopic examination) is a part of my diagnostic workup.
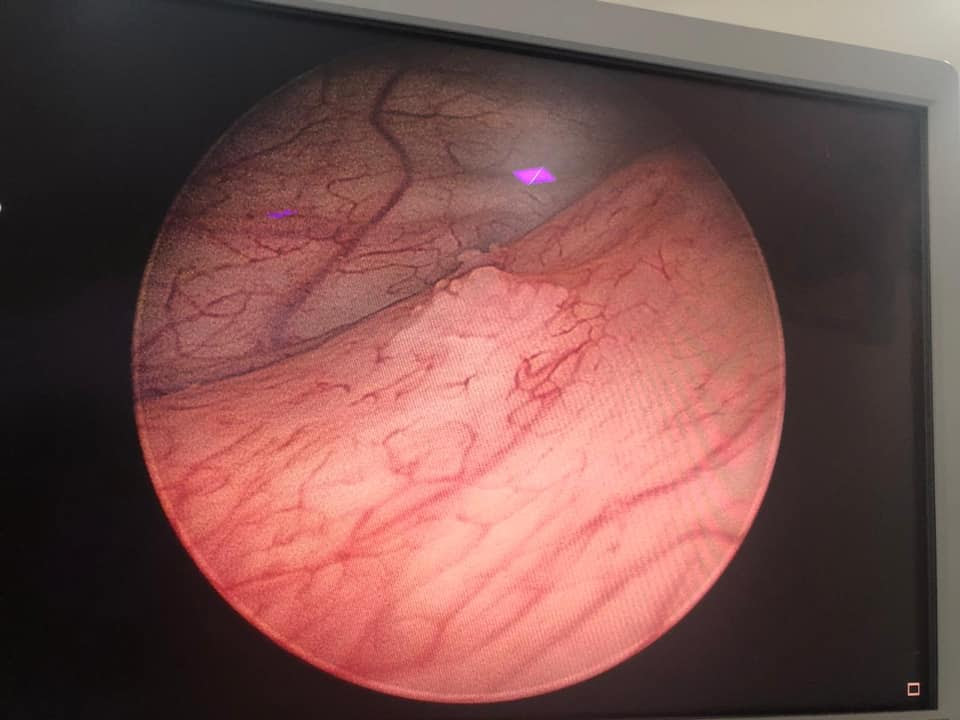
Cystoscopy allows urologist to examine the lining (surface) of urinary bladder and the urethra (water pipe), which is a tube carrying urine out of body. It can be done in a special room, using a local anaesthetic jelly (numbing jelly) or sedation or under general anaesthesia in the hospital. I generally take into account patient’s preference and the availability of the equipment by the hospital. It also depends on the reason for the procedure.
In case of bladder cancers, specially CIS (Carcinoma in situ), which is a high grade non muscle invasive bladder cancer, 20% of them could be associated with OAB symptoms. It isn’t vice a versa but it is very important to rule out any underlying bladder conditions which could contribute to the symptoms of OAB. So far, I have found bladder cancers in such patients, squamous metaplasia, multiple types of cystitis including follicular cystitis.
One of my patients recently had squamous metaplasia on cystoscopy and biopsy. There are 2 types of it, non-keratinised, which is benign type and the keratinised which is a premalignant condition (can turn in to cancer) hence needs regular cystoscopic follow up. Apart from diagnostic purpose I also use it therapeutically by doing cystodistension wherever it is necessary.
Surgery is not a solution for every problem. Yes, in case of failure of medical treatment surgery or interventional procedures. For overactive bladders my preferred option is always to treat with lifestyle changes and with medications first. I try to keep surgical option away as much as possible. I investigate them thoroughly and accurately. When the condition is refractory to medical treatment, I then have thorough discussion with patient as well as their family members, explain them risks Vs benefits of the surgical intervention and then proceed with the surgical option. I always adopt patient centred approach and help the patient as well as relatives to make informed decision.